Hernia Surgery
Contents
Overview of Hernias
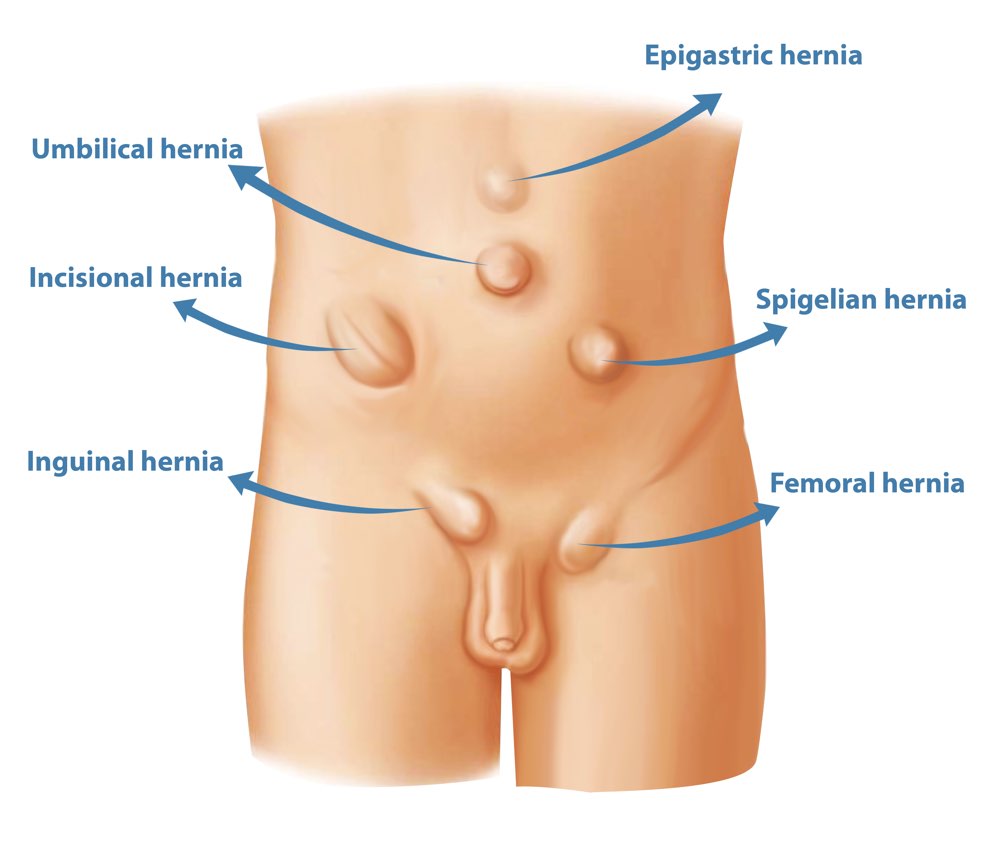
Different Types of Hernia
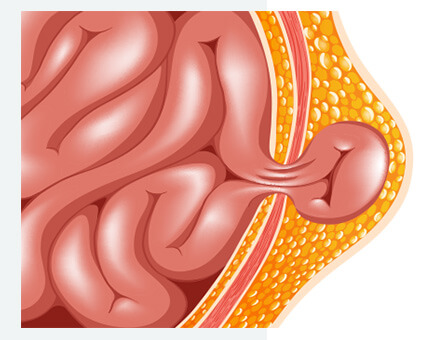
A hernia is a weakness or opening in tissues or muscles that allow the bulging of its contents. Most often, this is when there is an opening in the abdominal wall that allows your abdominal contents (intestine, fat, organs) to bulge through.
“ING-gwuh-nal” this is the most common type of hernia that happens in the groin, when fat or intestines bulge through a passageway in the thigh – the “inguinal canal”
A more rare type of hernia that happens lower in the groin, when fat or intestines pass below the inguinal ligament at the groin fold
Another very common type of hernia at the belly button, which are mostly present at birth (congenital)
Hernias that occur anywhere there has been a previous incision where the closure weakens over time. This can happen in up to 10 – 15% of patients who have any abdominal incision.
Hernias that occur on the front surface of your abdomen. This is a general term that includes umbilical hernias, incisional hernias, or epigastric hernias (which occur above your belly button)
A hernia that occurs next to a stoma – when a piece of intestine is brought up to the skin surface after a surgery (ileostomy, colostomy, urostomy, etc). Since this is a man-made opening in the abdominal wall, all stomas will eventually develop parastomal hernias with enough time and strain, but not everyone develops symptoms or need surgery.
A common type of hernia that happens when the natural opening in your diaphragm where your esophagus (feeding tube) passes through widens. This might allow your stomach or other organs to pass through into your chest causing discomfort or gastric reflux. Most patients don’t have any symptoms and this is found by chance on an imaging scan. However, if it is causing symptoms, you may be offered a surgery.
A rare type of hernia that pushes between some of the layers of the abdominal wall, but doesn’t completely protrude through all the layers. For this reason, there’s often no obvious bulge and it is harder to detect. It often happens below the belly button at the lateral border of your ‘abs’.
A rare birth defect where the diaphragm doesn’t close during a baby’s development. Sometimes, this can cause problems with lung development.
How common are hernias?
This depends on the type of hernia, but in general hernias are very common. Roughly 1 in 3 men or people assigned male at birth are diagnosed with an inguinal hernia whereas roughly 1 in 25 women are diagnosed with an inguinal hernia. (1)
Umbilical hernias are found in 30 – 50% of people in the general population, but only 15% of people with umbilical hernias undergo surgery. (2)
Incisional hernias occur in roughly 10-15% of people who have an abdominal incision (3).
What causes hernias?
Many factors can play into the development of hernias:
- A weakness in the abdominal wall:
- from a birth defect (belly button)
- from a previous surgical incision
- from natural openings that can get wider (e.g. around the esophagus, the inguinal canal in the groin)
- Excessive straining of the abdomen:
- obesity
- straining, heavy lifting, sports
- persistent coughing
- pregnancy
- Medical conditions that affect the strength of your tissues and wound healing
- diabetes
- smoking
- steroid use or other medications
- connective tissue disorders
Symptoms and Diagnosis
What are the symptoms of hernias?
Many hernias don’t cause any symptoms and may be incidentally found on a routine scan.
The most common symptom of an abdominal hernia is a bulge that appears or grows larger with standing, coughing, straining or heavy lifting. This bulge can cause very little symptoms at first, but may cause pressure, aching, or pain.
You should be able to push a hernia back in by lying down, relaxing your abdomen, and applying gentle pressure. If you suddenly can’t push your hernia back in and it is become more tender and painful, go immediately to the emergency department or call 911. Some people have hernias that get so large over a long period of time that they cannot be pushed back in.
More rare symptoms might be constipation, urinary discomfort/difficulty, or numbness and tingling in the groin or scrotum.
When should I go to the emergency department?
Emergency symptoms of a hernia include a hard tender bulge that you suddenly can’t push back in, severe pain, fevers, nausea and vomiting, and/or inability to pass gas and stool. If any of this happens, go immediately to the emergency room or call 911. This can happen if the intestines or other organs are trapped in the hernia causing a bowel blockage or even the intestines to be choked off.
The risk of developing a hernia emergency for most patients is <1% per year.
If you suddenly have a painful lump, fevers, nausea and vomiting, or you are unable to pass gas and stool, go to the nearest emergency department go call 911.
How are hernias diagnosed?
Most hernias are diagnosed by a physical examination by a doctor. Some hernias may require imaging like an ultrasound or CT scan to confirm the diagnosis or for planning your surgical approach.
Keep in mind not all hernias seen on imaging need to be fixed – see “When should I get my hernia treated”.
What are things commonly mistaken for hernias?
There are a lot of things that are mistaken for hernias, but aren’t true hernias and are treated quite differently.
A sports hernia is a misnomer, and not a hernia at all. It is a general term for groin pain caused by a number of different issues, but most commonly a tear or strain of a muscle or tendon in the groin. However, there is no weakness or opening through which intestinal contents can bulge through. As well, these do not require a hernia surgery per se, and can be managed a number of different ways including rest, physiotherapy, pain management, and muscle/tendon/joint surgery.
Diastasis Recti (diastasis rectus abdominus, rectus diastasis, abdominal separation) is a separation of the rectus abdominus muscles (the ‘abs’). This can cause a weakness in the middle of your abdomen and can cause a bulge to appear. This can be congenital but most commonly happens to about 60% of patients after pregnancy. For most people, the diastasis will go away.
As rectus diastasis isn’t a true hernia and doesn’t have the risk of a choking off intestinal contents, surgery isn’t mandatory. Physical therapy, weight loss, and exercise works for the majority of patients. For patients who have the significant symptoms caused by the diastasis, or for those who are cosmetically bothered by its appearance, surgery can be considered.
These are all scrotal processes that can often be mistaken for hernias.
Spermatocele – a non-cancerous fluid-filled growth that develops from the epididymis – the tube that transports sperm from the testicle. These are managed by urologists if they cause symptoms.
Varicocele – a swelling of the veins in your scrotum, which can affect fertility in some people. These are managed by urologists.
Hydrocele – a benign buildup of abdominal fluid in the scrotum. Often people are born with a persistent communicating channel between the abdomen and scrotum (patent processus vaginalis) that causes build up of fluid. These often cause no symptoms and don’t need to be treated, but can be treated by a urologist.
Patients may have nerve injuries from previous abdominal incisions or from viruses (e.g. herpes zoster – shingles) that cause a denervation and weakness of the abdominal wall muscles, leading to bulging. However, this is not a true hernia and often does not require surgery.
There are bulges that can be caused by benign and malignant abdominal wall masses. These can be best diagnosed on physical exam and with imaging by your doctor.
Management and Treatment
What is the treatment for hernias?
Aside from umbilical hernias in infants, which often resolve by school age, there are very few hernias that will get better on their own. Small hernias that cause little to no symptoms can be managed without surgery with a “watch and wait” method to see if the symptoms get more bothersome. Some hernia symptoms can be managed with binders or trusses. Since most hernias get larger with time and cause more discomfort or symptoms, most hernias are fixed with surgery.
Who treats hernias?
Hernias are often diagnosed by family doctors and referred to general surgeons for treatment. General surgeons may take on a hernia or refer to another surgeon depending on the type of hernia, the complexity, and their experience/scope of practice. Certain hernias may require subspecialty general surgeons including:
- Foregut/bariatric/minimally invasive surgeons or thoracic surgeons – manage hiatal hernias
- Abdominal wall reconstruction surgeons – manage complex or rare hernias, massive hernias, or redo hernia surgery
Should I get my hernia treated?
Whether you get your hernia treated or not depends on:
- the type of hernia
- whether it is causing you any symptoms
- whether it has the risk of causing future problems
- If you have a hernia that can be fixed, that is causing symptoms, or has a risk of causing future problems, your surgeon may recommend surgery for you and discuss your options.
- Your surgeon may recommend a “watch-and-wait” approach for hernias that don’t cause any symptoms or minimal symptoms, particularly small hernias seen on an ultrasound that can’t be felt on a clinical exam. Since hernias do tend to worsen over time, most abdominal hernias are fixed with surgery.
- Umbilical hernias in babies and infants can go away on their own. Your surgeon may recommend watching to see if this goes away before school age.
- Hiatal hernias often don’t cause any symptoms and are found by routine imaging or while investigating for something else. However, if they do cause symptoms like chest discomfort or gastric reflux, surgery may be recommended.
If you are showing signs of a hernia emergency – severe pain, fevers, vomiting, or an irreducible bulge – you need to call 911 and go to immediately to the emergency department.
What happens if I don’t get my hernia fixed with surgery?
You can live a long time with a small hernia that causes little to no symptoms. Hernias in general do get larger over time and cause more symptoms, leading patients to pursue surgery.
For patients who choose not to have surgery or to wait until the future to see if you develop worsening symptoms, we suggest continuing to live your life without any exercise or activity restrictions. You might decide to wear a truss or abdominal binder to help manage your minor symptoms.
For patients who cannot have surgery because surgery isn’t feasible, speak to your surgeon about strategies to manage your symptoms.
References
- Kingsnorth A, LeBlanc K. Hernias: inguinal and incisional. The Lancet. 2003;362(9395):1561-71.
- Bedewi M, El-Sharkawy M, Al Boukai A, Al-Nakshabandi N. Prevalence of adult paraumbilical hernia. Assessment by high-resolution sonography: a hospital-based study. Hernia. 2012;16:59-62.
- Nachiappan S, Markar S, Karthikesaligam A, Ziprin P, Faiz O. Prophylactic mesh placement in high-risk patients undergoing elective laparotomy: a systematic review. World journal of surgery. 2013;37:1861-71.
- Moon V, Chaudry GA, Choy C, Ferzli GS. Mesh infection in the era of laparoscopy. Journal of Laparoendoscopic & Advanced Surgical Techniques. 2004;14(6):349-52.
- Kuo Y-C, Mondschein JI, Soulen MC, Patel AA, Nemeth A, Stavropoulos SW, et al. Drainage of collections associated with hernia mesh: is it worthwhile? Journal of Vascular and Interventional Radiology. 2010;21(3):362-6.
- Öberg S, Andresen K, Klausen TW, Rosenberg J. Chronic pain after mesh versus nonmesh repair of inguinal hernias: a systematic review and a network meta-analysis of randomized controlled trials. Surgery. 2018;163(5):1151-9.
- Itani KM. New findings in ventral incisional hernia repair. JAMA. 2016;316(15):1551-2.
- Lorenz R, Arlt G, Conze J, Fortelny R, Gorjanc J, Koch A, et al. Shouldice standard 2020: review of the current literature and results of an international consensus meeting. Hernia. 2021:1-9.
- Desarda MP. New method of inguinal hernia repair: A new solution. ANZ journal of surgery. 2001;71(4):241-4.
- Lockhart K, Dunn D, Teo S, Ng JY, Dhillon M, Teo E, et al. Mesh versus non‐mesh for inguinal and femoral hernia repair. Cochrane Database of Systematic Reviews. 2018(9).
- Stabilini C, van Veenendaal N, Aasvang E, Agresta F, Aufenacker T, Berrevoet F, et al. Update of the international HerniaSurge guidelines for groin hernia management. BJS open. 2023;7(5):zrad080.
- Rosenberg J, Bisgaard T, Kehlet H, Wara P, Asmussen T, Juul P, et al. Danish Hernia Database recommendations for the management of inguinal and femoral hernia in adults. Dan Med Bull. 2011;58(2):C4243.
- Simons M, Aufenacker T, Bay-Nielsen M, Bouillot J, Campanelli G, Conze J, et al. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Springer; 2009. p. 343-403.
- Anthenelli RM, Benowitz NL, West R, St Aubin L, McRae T, Lawrence D, et al. Neuropsychiatric safety and efficacy of varenicline, bupropion, and nicotine patch in smokers with and without psychiatric disorders (EAGLES): a double-blind, randomised, placebo-controlled clinical trial. The Lancet. 2016;387(10037):2507-20.
